I’ve been slacking with creating new content for the past few months, its been difficult to find the motivation sometimes especially when one is dealing with a million other things. But now with this pandemic going on, countries are facing global lockdowns and being a dermatologists and not someone working in the front lines of this health crisis, I now have more time to dedicate to this blog again. And I hope you’re all safe and well wherever you are.
As my first posts in months, I’ve decided to share something more on a personal note and not too much of the normal “science behind skincare” content I normally post.
I was lucky enough to be able to have a wedding reception in Goa recently in February 2020, just before this pandemic shook the world by storm.
I’ve been requested to share by professional advise on skin care for the upcoming brides out there. I was honoured to be featured by https://hitchedhaven.com/ (a website catering to future brides & grooms seeking to tie the knot in goa) on their website about my skincare advises as a dermatologists for “that wedding glow”.
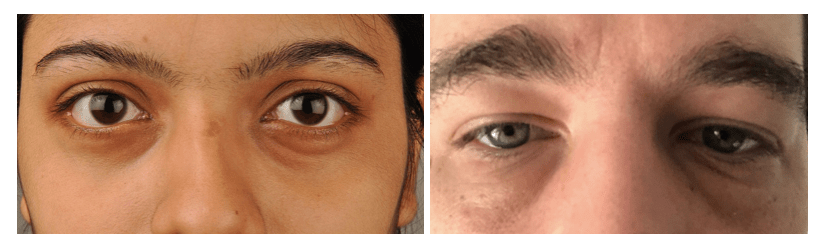
Here are some pictures without makeup.
And the pictures from the wedding:
As a dermatologist skin care is my expertise. I’m a firm believer and advocate of evidence based consistent skin care regimen which means I use products backed up by science and I do not resort to DIY or home remedies for my skin or hair.
You plan for your wedding months ahead, similarly your skin needs the same amount of attention months prior to the big day.
Seek a consultation with a dermatologists to help formulate a skin care routine addressing your personal issues (be it acne, or pigmentation etc). Its important to start this early as there is no “fast track treatment” for such issues yet except for the magic of makeup, which can conceal anything. But if you’re someone like me who does not like wearing too much makeup and want to keep things as subtle and natural as possible then:
Find a dermatologist before you find a makeup artists.
If hydrated, clear, glowy skin is your goal without having to worry about the thick layer of makeup on your face for your wedding day especially if you’re planning to have a destination wedding in the humid climate of goa, here are some advises for you:
- Use a broad sunscreen with both UVA and UVB protection. Search for one with spf 30 and above with a PA factor of +++, this will help prevent sunburns and tanning which makes your skin look dull. If you want help with your choice of sunscreen, check out my previous post: https://drnaphi.com/2019/07/15/all-about-sunscreens/
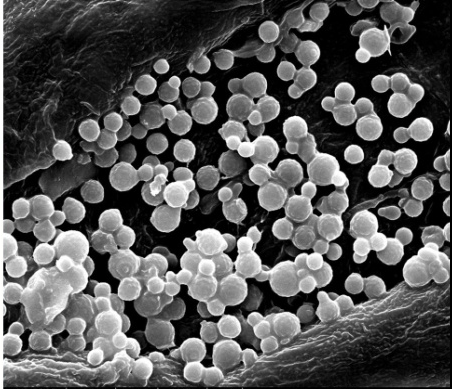
- You may opt for sessions of chemical peels which helps with pigmentation and gives you a glowy youthful skin. Chemical peels are out patient procedures performed by certified dermatologists in their clinics. Higher strength acids such as glycolic, salicylic, or trichloroacetic acids etc are used in multiple sessions of 2-3 weeks apart, to help achieve a clearer skin.
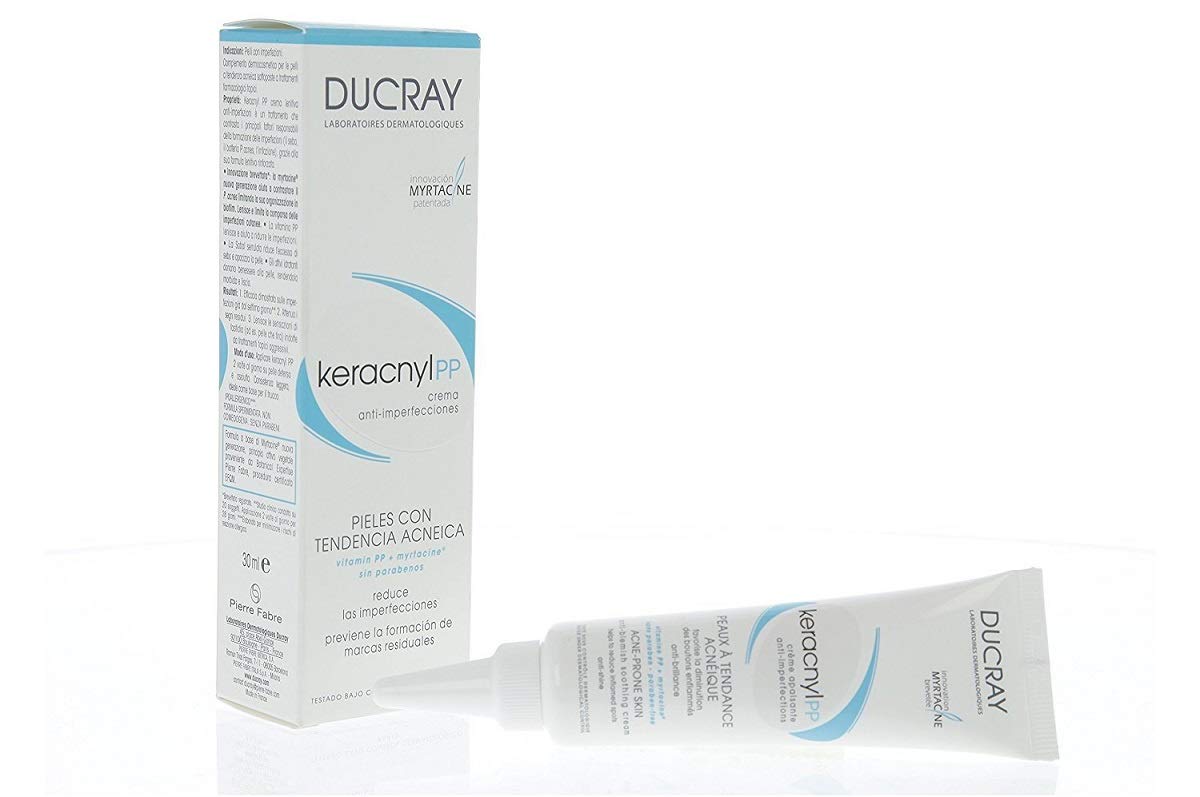
- Always use a moisturiser. And yes, you still need a moisturiser even if you have oily acne prone skin, and its especially important if you’re using an active ingredient for your acne such as retinoids, benzoyl peroxide etc. I have acne prone skin and below are some of my favourite moisturisers:
- Facials, clean ups are optional, but if you want that extra layer of pampering, then don’t wait till the day before to do it. The reason being, in case you do experience some allergic reactions from any of these products, your skin will have the time to heal. Do it a week before the big day and maybe just use face mask sheets for the instant hydration the night before.
Your skincare does not end on your wedding day.
Remember to wash your face thoroughly after the celebration. I know you’re going to be tired after at the end of the night but trust me, you need to get that makeup and sweat from the entire day off your skin before you take your final rest.
Use a micellar water or cleansing oil as the first step to remove all the oil based makeup. Then clean your face with any cleanser after.
My go to micellar water, but there are so many other versions out there in the market. You can use any one of your liking.
Cleansers I swear by, and its not just for this special day, I use them on a regular basis.

Cereve hydrating cleanser 
LaRoche Posay toleraine creme cleanser
Lastly, moisturise and enjoy your wedding night 🙂