How many times have you tried an anti-aging or anti-acne creams or a brightening serum but failed to see it work on you?
Your constant breakouts never stopped, the mirror reflects back new wrinkles and your pigmentation is stubborn enough to never fade.
I’ll be the first to admit, I’m definitely guilty of the above!!
I grew up with acne as a teenager which continued into my adulthood. I’ve tired over the counter creams and in the early 2000’s “Erytop” (clindamycin – an antibiotic cream) was widely available. All my friends were using it. It would work for the existing pimple but news ones were popping up constantly. My mum did take me to a dermatologist then, I would get prescribed one cream- benzoyl peroxide and was advised “apply it once at night” and that was it. I was never explained how long I should be using it for, what cleansers I should be using, nor was I explained about the potential side effects or the expectations one should have with such topical medication.
And it seemed quite normal then, go for that one time consult for acne and the dermatologist would assure my worried mum that “your daughter will grow out of it, the acne will subside when her teenage years have passed”.
This might have been true for older generations but now with the changes in lifestyles, acne persisting into adulthood is quite common. Teenagers suffer from a more severe form of acne with the potential for permanent scarring.
The same holds true for pigmentation issues particularly melasma. Women, though bothered by the facial pigmentation, DIY remedies or creams suggested by their friends were enough to make them feel like they are actively taking care of their skin.
Things are different now. Individuals are more aware through social media about how to care for their skin. Educational content are more accessible about the various skin or hair issues. And skin care products are easily available at the touch of a button.
I personally love to see this change.
How to achieve the best from your skin care?
Skin care is actively caring for your skin (be in for acne, pigmentation, ageing or just general measures) to maintain a healthy looking skin.
Some people can follow multiple steps layering different skin care products both day and night for their skin and this may work wonders for them, but a simple basic routine is also not wrong.
If you have a particular concern I strongly advised seeing a dermatologist for any skin problems.
Before seeing a dermatologist, prepare yourself with the questions you would like to ask. Do not be afraid to clear your doubts. I always advised my patients who are already on treatment for some other condition or who are already on some form of skin care regimen to bring all the medications (both oral-tablets, capsules and topical- creams, ointments, serums) during their consultations.This is because few medications may be contraindicated with the medications that I may prescribe, or maybe the skin rash is actually associated with the medication they are taking. And in India, it is very common to see patients applying the wrong cream for the wrong reason or to the wrong site.
Always remember to tell your treating doctor if you are allergic to any medication or if your skin is sensitive to any skin care product.
Once a diagnosis of your condition is made, try to understand the condition, either by asking your doctor or reading up more about it yourself. Its always helpful to know why it happens, is it curable? how to manage it? how to prevent it from recurring? etc.
Skin care routine is not a static process. It changes depending on the response, the season, the tolerability of a person to an ingredient in a product, the availability of the products, the age or pregnancy status or according to the money and time one is willing to invest in it.
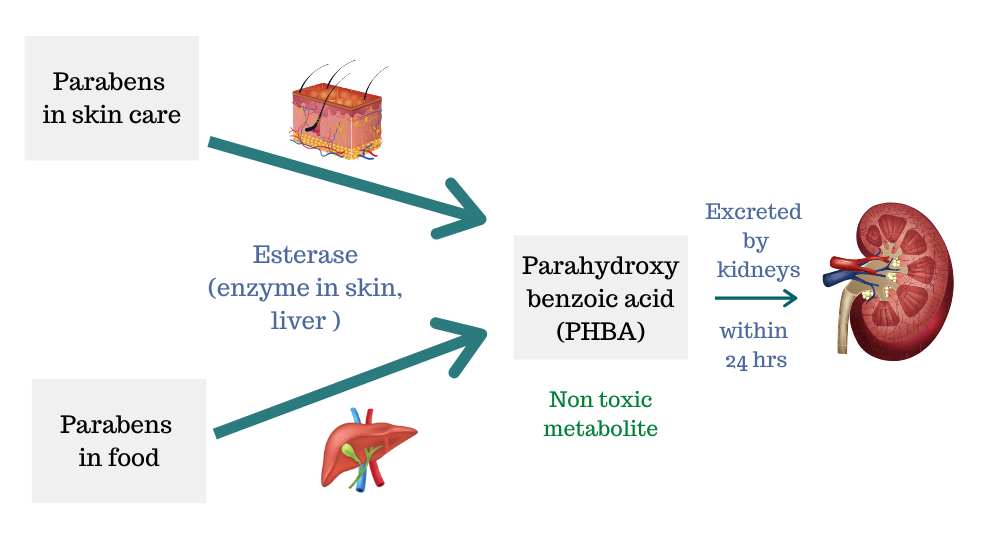
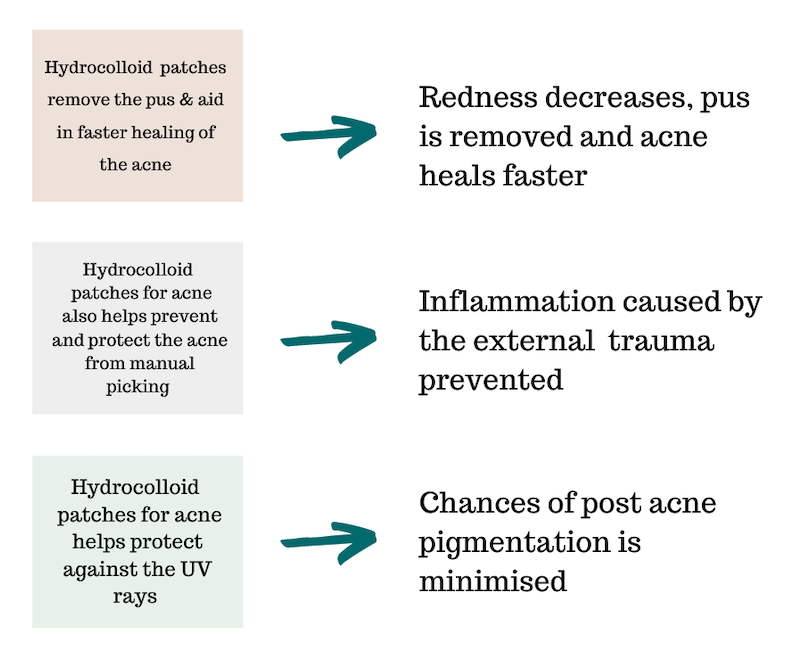
Once a diagnosis is made and a skin care routine is advised, understanding the ingredients in the products is just as important. Its good to know how a product works, how you need to be using it, how to minimise side effects and how long it takes for the product to work.
Most times when people blindly follow the doctor’s advise or a beauty influencer without understanding the product, it either leads to development of side effects, lack of results, pre-mature discontinuation of the product or maybe even worsening of the condition.
Always follow up as and when your dermatologist advised or earlier if needed. Follow up consultations are as important as your first visit. This is when your dermatologist can assess how you are responding to the treatment and if the products need to be changed based on your response. Your dermatologist will even be able to help you manage the side effects if any.
Be patient. Consistency is the key with skin care. Avoid doctor and product hopping too early and frequently. Most ingredients in skin care products take at least 4-8 weeks to start showing effect.
Avoid using too many active ingredients at once especially if you are a newbie.
Be gentle, go slow, skin care is a personal journey and not a competition.
Try to have more realistic expectations. One may never be acne free forever, even with the right skin care, you may get the occasional breakouts, and thats OKAY. Pigmentation can slowly fade with time and anti ageing cream can help reduce those fine lines but your skin will never go back to the skin you had in teenage years.
Lastly, change your perspective about skin care. Do not see it as a burden and a waste of your time. Instead keep in mind that you are actively taking care of your skin and enjoy doing it.
Hope these tips help you achieve the maximum with your skin care routine.